Find this recipe and more in our cookbook, Complete Month of Meals, where you can mix and match recipes to make meal planning easy! To order directly from the American Diabetes Association, click here.


Find this recipe and more in our cookbook, Complete Month of Meals, where you can mix and match recipes to make meal planning easy! To order directly from the American Diabetes Association, click here.

Quick answer: There isn’t one. At least not one exact diet that will meet the nutrition needs of everyone living with diabetes. Which, in some ways, is unfortunate. Just think how simple it would be to plan meals if there were a one-size-fits-all plan that worked for everyone living with diabetes, prediabetes, or at risk for diabetes. Boring, yes, but simple!
As we all know, it’s much harder than that. We don’t often make food choices based on nutrition science alone —we often also make food choices for social, cultural, or emotional reasons. And because each of us is different, we each need to find an eating plan best matches both our nutrition and lifestyle needs.
For people living with diabetes and trying to learn more about healthy food choices, it can be tough to tell fact from fiction and make decisions in a sea of choices. Information in the news can often be confusing, with conflicting data and advice often given at the same time.
Part of our job at the American Diabetes Association is to help sort out the science and provide guidance that is safe and works well for people at risk for and living with diabetes. And current research shows there are a many eating patterns that can work to maintain a healthy life with diabetes, not just one. In the long run, an eating plan that you can follow and sustain and that meets your own diabetes goals will be the best one for you.

A meal plan takes into account your likes, dislikes, and lifestyle. It is a guide that is aimed at helping you meet your personal weight and blood glucose goals and guides you on what, when, and how much to eat. While many people may think a meal plan is the same as a diet, we like to consider a meal plan as something you follow over time rather than a diet, which is often related to a quick fix for a short period of time.
We often make food choices for social, cultural, or emotional reasons
An eating pattern is a term used to describe the foods or groups of foods that a person chooses to eat on a daily basis over time. There a number of eating patterns that are helpful for people living with diabetes or at risk for diabetes. Following are a few of the more popular choices that the science shows can work. You’ll notice that all of these have three things in common:
There is no “one-size-fits-all” eating plan or “ADA Diet” for people with diabetes! The best eating plan for you is the one that you can sustain while still meeting your diabetes goals.
Mediterranean-style eating uses olive oil as the main source of fat. Fish, chicken, and small amounts of dairy products, such as cheese and yogurt, are included. Red meat is less common, though wine can usually be consumed in small amounts (one to two glasses of wine per day) with meals.
There is a lot of research on the Mediterranean style of eating and most of it shows it may help you improve blood sugar, lose weight, and reduce risk of heart disease, stroke, and some cancers. This is a well-studied eating pattern than can work for many people with diabetes.
There is no “one-size-fits-all” eating plan or “ADA Diet” for people with diabetes!
Vegetarian eating plans generally include nuts, seeds, beans, and meat substitutes with little or no animal

products, though there are many eating patterns you could label “vegetarian.” These patterns are different in terms of protein sources, from vegan eating plans that include no animal products of any kind to new patterns, such as flexitarian eating plans that include mostly plant-based foods but allow for eating meat at times.
A low-carbohydrate (low-carb) eating plan includes protein foods like meat, chicken, fish, shellfish, eggs, cheese, nuts and seeds, and fats (oils, butter, olives, and avocado). Most low-carb plans, such as Atkins, Keto, and Paleo, avoid highly processed carbohydrate foods and grains.
DASH is an acronym for “Dietary Approaches to Stop Hypertension” and began as a research study to help lower blood pressure in people with hypertension (high blood pressure). This eating plan limits foods high in sodium (salt), saturated fat, red meat, sweets, added sugars, and sugary drinks.
Try the Diabetes Plate Method. Most of the eating patterns above focus on what to eat. The Diabetes Plate Method helps figure out how much to eat, which can often be just as important. It takes the burden out of measuring and counting while meeting the goals of many of the eating patterns described above. This method uses a 9-inch plate, often a smaller plate than most people use. Once you have a smaller plate, the idea is to fill half your plate with non-starchy vegetables, 1/4 of your plate with protein foods, and the last 1/4 of your plate with carbohydrate foods.
Try to block out the fad-diet advice and choose a plan you are likely to follow long-term that fits both your diabetes goals and your personal needs. Think about your likes and dislikes and how a change to your eating will affect your day-to-day life with family and friends. Then see how you can match this with your personal weight-loss goals. Budget also plays a part in choosing the right healthy eating plan that will meet your needs.
Many eating patterns can help you maintain a healthy life with diabetes.

Eating foods that have vitamins, minerals, and other nutrients and are minimally processed will help you reach your health goals. Foods like whole grains, vegetables, fruits, lean poultry, seafood, plant proteins, heart-healthy fats, and low-fat dairy have lots of nutrients with fewer calories. Eating these types of food will help you keep your kidneys healthy, manage diabetes, and lower your risk for other health problems. If you have CKD, you may need to limit foods with potassium and phosphorus—talk to your doctor or registered dietitian nutritionist (RDN) to find out.
Eating minimally processed foods also helps lower the amount of sodium you eat each day and stay within recommended levels. If you’re eating packaged food, choose foods that are labeled as low-sodium, no-added salt, or no-added-sugar. Your health care team will let you know if you need to limit your intake of certain foods to keep your nutrient levels within normal limits.
If you need to manage your phosphorus and potassium intake, you can work with your registered dietitian nutritionist to help you adjust your eating plan. The first step is to avoid be cautious of highly processed foods that have phosphorus and/or potassium additives by looking at the ingredient list and looking at the potassium and phosphorus levels written on the nutrition facts label. These can add significant amounts of phosphorus and potassium to your diet. Naturally occurring foods with potassium and phosphorus also need to be monitored. However, understanding some fruits, vegetables, meats, dairy, nuts and legumes can have higher levels, but our body absorbs these nutrients differently. By making changes to your eating plan, you can still enjoy a variety of foods while working toward your health goals.
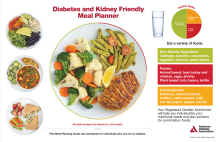
One effective tool for planning meals is the diabetes- and kidney-friendly meal planner, which helps you plan meals with balanced portions for a nourishing eating pan. Here’s how to use it.
Start with a 9-inch plate.
Fill half your plate with non-starchy vegetables. For those with CKD who need to limit their intake of phosphorus and potassium, choose options that have essential vitamins, minerals, and fiber. Examples include:
In one fourth of your plate, add starchy vegetables or grains. Starchy vegetables and grains will affect your blood glucose most but provide you with energy and nutrients. Choose whole grains when you can to be able to get more fiber in your meals. Examples include:
The last one fourth of the plate, add proteins. Choose lean animal-based and plant-based proteins for lower calories and fats. Eating the right amount of protein in your meals is part of managing CKD. By eating the right amount of protein, you can help keep your kidneys from working too hard after meals.
Plant-based proteins have been shown to reduce health complications and support kidney health. Including a variety of protein sources in your eating plan will help you get essential amino acids
Examples of lean proteins include:
Eating heart-healthy fats and limiting saturated fats helps with kidney and heart health. Aim to include omega-3 fatty acids and monounsaturated fats in your meals. Examples of healthy fats include:
While water should be your first choice to drink, you can also drink no-calorie options. Some examples are flavored water, unsweetened coffee, unsweetened tea, or zero-calorie clear (not dark) carbonated drinks.
Having diabetes and kidney-friendly eating plan will help you manage diabetes and CKD. By using the diabetes- and kidney-friendly meal planner,, you can create balanced, nourishing meals that support your health. You can also talk with your registered dietitian nutritionist (RDN) to create an eating plan built for your specific needs and goals.
For more resources on diabetes and kidney disease visit diabetes.org/kidney.

This article is brought to you by DaVita, National Sponsor of Living with Diabetes.

Are you looking to eat more plant-based meals and reduce the amount of red meat in your diet? Research continues to show that people who regularly eat red or processed meat are at an increased risk of heart disease, stroke and type 2 diabetes. Additionally, red meat can be expensive at the grocery store.
Reducing red meat intake has many benefits, including protecting your heart and overall health and lowering your spending. Read on to learn how you can take the focus away from red meat and let plants shine.
Instead of giving up red meat all at once, how about starting slow with small steps? There are a few approaches you can take, such as:
Here are some ways to reinvent dishes that focus on ingredients other than red meat:
Ready to start your plant- based cooking adventure? Be sure to check out all the recipes on Diabetes Food Hub and create an account so you can save plant-based recipes to try later. You can even create and print a grocery list to bring with you to the grocery store!

Meal planning and cooking when managing diabetes can be easy and you can still enjoy your favorite foods. With a few food substitutions or a change in the cooking method, almost any dish can be diabetes-friendly.
We’ve put together some easy food substitutions for healthier meals you can apply to new recipes or old favorites.
Non-Starchy Veggies
Carbs have the biggest impact on blood glucose (blood sugar). An easy way to cut back on carbs (like pasta, rice, and potatoes) is by swapping them for non-starchy vegetables or vegetable-based alternatives.
There are many great low-carb options at most grocery stores, such as:
Lean Protein
Protein is an essential nutrient for your body because along with other benefits, it helps build and repair tissue and muscle. However, high-fat protein sources, like pepperoni and bacon, contain unhealthy saturated and trans fats that can raise your risk for heart disease. Get the benefits of protein from lean sources that contain fewer unhealthy fats. Try to use protein foods such as:
Try to choose red meat less often than white meats and fish. If you are shopping for red meat, look for at least 90% lean varieties such as:
Another healthy option is to choose plant-based proteins for your eating plan. Lean plant-based options include:
Low-Fat Dairy
Dairy fits into a healthy eating plan, but it’s important to know that many dairy products have high-fat content. Try to choose low-fat dairy products. Healthy sswaps for full fat dairy products:
Remember that most dairy products have carbs, so be sure to include them in your daily carb count. And while cheese is a dairy product, it falls into the protein section of our Diabetes Plate. Choose a low-fat variety of cheese as a very low- or no-carb protein source.
Healthy Fats
Solid fats (like butter and coconut oil) are solid at room temperature and liquid fats (like olive and avocado oil) are liquid at room temperature. In most cases solid fats are high in saturated and trans fats, so try not to use them. You can cut back on solid fats by choosing fats such as:
This change will usually work in cooking (making chicken, pasta, etc.), but may not work when baking (making cakes, cookies, etc.). Check the label to see if the product will work for what you’re making.
Whole Grains
Carbs are part of the Diabetes Plate and are an important part of healthy eating plans with the right serving size. But some carbs (typically what we consider refined grains, such as white bread) aren’t the best energy source for managing your blood glucose (blood sugar) levels. Try substituting white bread with whole grain sources which have less impact on blood glucose levels. Some delicious and easy swaps include:
Spices
While salt is a part of many recipes and important to our health, it can affect blood pressure. Think of cooking as a great time to experiment with different herbs, spices, and other ways to add flavor without salt! Try using:
Sweeteners
Low calorie or non-nutritive sweeteners are a great option for sweetening your food and drinks with the least amount of carbs or calories. These have very little impact on your blood glucose. Some alternatives you can find in the store are:
Sweetening your food with honey, agave, and maple syrup instead of sugar isn’t the best way to replace sugar because they contain carbs and calories and quickly raise your blood glucose.
If using these alternative sweeteners in baking, make sure you’re using the right amount. If a recipe calls for one cup of sugar, you may not always swap it with one cup of an alternative sweetener. Typically, the sweetener’s company will list the amount needed to replace white sugar on its package.
The Bottom Line
Finding healthy substitutions that work in your recipes will make them healthier and easier to fit into your eating plan! After a while, you will get into the swing of things and figure out what works and tastes best for you.

Visiting the farmers market is a different experience than going to a standard supermarket. Here are eight tips to help you know what to bring and make the most of your access to farmers’ and artisans’ fresh products and knowledge!
Most of all, have an open mind on your trip. A farmers’ market is a great way to find and try new types of produce and you can prepare meals with fresh produce that’s in season.
Be aware of what fruits and veggies are in season to enjoy your favorites when they’re fresh. You may find that what you buy at the farmers market inspires you to create new, flavorful, and healthy dishes. Don’t forget to sign up for Diabetes Food Hub’s e-newsletter for diabetes-friendly ideas and recipes using your fresh new produce!

We all know eating veggies is good for us—their fiber alone can help you manage your weight and heart health. You’ll find two types of vegetables at the store: starchy vegetables (like peas, potatoes, and corn) and non-starchy vegetables (like broccoli, eggplant, and peppers). While all vegetables offer important nutrients for people with diabetes, you should aim to fill half your plate with non-starchy vegetables for a balanced meal that doesn’t spike your blood glucose (blood sugar).
With all this in mind, eating the same veggies in the same way every day can often become boring. Keep reading for some quick tips on how to cook veggies the diabetes-friendly way and try something new to keep things interesting.
The beauty is that all three can be part of a healthy eating plan. Many enjoy the taste and texture of fresh veggies, especially when they’re in season. However, many fresh veggies require you to use them quickly or they’ll spoil. On the flip side, frozen and canned options offer convenience and a longer shelf life, and they have been picked and packaged at their peak of freshness.
Frozen and canned vegetables may have added ingredients that could increase their sodium and fat amounts. Look for frozen veggies that contain no ingredients other than the vegetable itself. When you prepare them, you can add your own flavorings, like herbs and spices. For canned varieties, choose no- or low-sodium options with minimal ingredients. Drain and rinse them before eating if the can contains sodium.
Different ways of preparing vegetables can bring out different flavors and textures. Here are some methods to test out in your kitchen and discover your favorite way of preparing veggies.
Set your oven to 425degrees F and plan to roast your veggies for 20 to 30 minutes depending on the vegetable and how well you like them cooked. Try cutting your veggies into 1-inch pieces as some, like carrots, beets, and potatoes, take more time to soften the bigger they are. Toss them with a healthy oil spray (like olive, canola, or avocado oil) and herbs and spices, and add them in a single layer on a baking sheet. Try cooking a pan of roasted veggies at the beginning of the week and use them in your meals over the next several days.
Pro tip: When roasting frozen vegetables, put your baking sheet in the oven while it preheats. Then you can add the vegetables to the hot sheet to help them cook and crisp up.
Steaming veggies (fresh or frozen) doesn’t require extra kitchen equipment, you can do it in your microwave! Using a microwave-safe dish, add your veggies along with two to four tablespoons of water. Every microwave is different, so start by microwaving for two to three minutes and increase as needed until your veggies are tender. Firmer vegetables like broccoli will need more time, but thin veggies like spinach will steam quickly.
Adding veggies to a hot skillet can be a simple but delicious prep method. First, heat up a little bit of oil with a high smoke point, like avocado, peanut, or canola oil. Next, add flavoring like diced onions or minced garlic and allow them to begin cooking before adding other veggies. Adding some water can help firmer veggies soften.
Pro tip: Veggies with shorter cooking times are green beans, asparagus, summer squash, and zucchini. Veggies with medium cooking times are broccoli, parsnips, and butternut squash. Long cooking times are more likely for cauliflower (unless it’s riced), Brussels sprouts, and potatoes. Add veggies with the longest cooking time to your skillet first and sauté for several minutes before moving to the medium and short cooking time veggies.
Bell peppers are the star of the show in this simple but flavorful dish. Packed with vitamins, bell peppers are a colorful way for a person with diabetes to add a touch of sweetness to a meal. Learn how to roast peppers quickly and easily with this recipe.
Garlic Sautéed Spinach and Kale
Are you not sure how to cook kale or spinach? Try this delicious and easy dish for a nutritious addition to your dinner. Leafy greens are packed full of vitamins and fiber and are low in calories and carbs.
Elevate your diabetes-friendly dining with these delightful Sautéed Thyme Mushrooms. Bursting with flavor and seasoned to perfection, these mushrooms are a tasty addition to any meal. Experience a dish that’s both satisfying and supportive of your diabetes management goals.

But the Mediterranean diet is also part of the Mediterranean lifestyle. This lifestyle includes being physically active, enjoying meals with others, and drinking water. For those that drink alcohol, having wine in moderation can be part of the lifestyle, too.
Following a Mediterranean lifestyle may play a role in improving insulin sensitivity and reducing the risk of developing type 2 diabetes and obesity. Plus, eating a Mediterranean diet may help with keeping your eyes healthy—namely vegetables, fruits, fish, and olive oil—may curb the risk of diabetes-related retinopathy.
For cooking with staples of the Mediterranean diet, a well-stocked pantry is key. Along with plenty of herbs and spices, plan to stock these eight delicious diabetes-friendly and nutrient-rich foods.
1. Extra-virgin olive oil
Using polyphenol-rich extra-virgin olive oil daily may improve metabolic control in people with overweight and type 2 diabetes. Swap in olive oil in place over other fats like butter or other oils.
2. In-shell pistachios
Pistachios are a great plant-based protein. Plus, they may play a role in reduction of fasting blood glucose and are delicious.
3. Tomatoes (can, carton, or jar)
Diced or crushed tomatoes, tomato sauce, and other tomato products, like marinara sauce, all provide lycopene. This naturally occurring pigment makes tomatoes red and may contribute to protection against diabetes and obesity.
4. Dry lentils
Compared to eating starchy foods like pasta, lentils seem to help lower post-meal blood glucose and insulin response.
5. Chickpeas (can or carton)
As part of a nutrient-rich, wholesome eating plan, research finds chickpeas may make it easier to manage your blood glucose thanks in part to their high fiber, protein, and low starch digestibility.
6. Bulgur wheat
Eating more whole grains, in general, is associated with a lower risk of developing type 2 diabetes, including insulin resistance, glucose regulation, and obesity.
7. Tahini (sesame seed paste)
Studies have found that consuming sesame products, including tahini, could have a beneficial effect on fasting blood glucose and A1C1 levels.
8. Balsamic vinegar
Due to its bioactive compounds and impact on the digestion process, balsamic vinegar may improve glycemic response to carb-rich meals.

The multitude of varieties can be overwhelming, especially knowing how to prepare them. Check out this list of the 8 winter squash you’re most likely to find in the store, and some ideas on how to prepare them.

Butternut: These are long with a bulbous end and a smooth tan skin. Because the skin is a little thick, you’ll want to peel them before cutting into chunks or dicing. Or, you can cut them lengthwise, remove the seeds, and roast them in the skin if to scoop out the flesh. Put these tips to action with this Butternut Squash and Kale Soup.

Honeynut: This is a smaller, sweeter version of the butternut with deeper orange flesh. It is about half the size of a butternut squash and a hybrid of butternut and buttercup squash. They are excellent when roasted with lots of herbs (think sage, thyme, rosemary), garlic, and just a bit of parmesan cheese.

Acorn: Don’t let the name fool you, this squash is not for the squirrels! You’ll love this sweet, petite green squash. Keep the skin on and slice into circles to grill or roast, Alternatively, you can slice in half lengthwise to stuff like these Stuffed Acorn Squash.

Delicata: These oblong squash are cream colored and have either green or yellow stripes. They are sweet and a perfect way to enjoy squash since they’re so easy to prepare. They can be sautéed, steamed, roasted, grilled, baked, or stuffed.

Green kabocha: These Japanese pumpkins are dense and sweet and usually deep green in color. Roast and turn them into soup with ginger, cumin, coriander, and garlic. Or slice and roast with olive oil, fresh ginger, thyme, and a little nutmeg.

Red kuri: Also called Hokkaido pumpkins, these little orange squash have a slight chestnut flavor, making them perfect for stews or side dishes in which they’re paired with other root veggies and some greens. Consider adding red kuri squash to this dish with fregola sarda and tahini dressing.

Sugar pumpkin: Unlike the larger jack-o-lantern pumpkins, sugar pumpkins are sweet and dense. They’re the pie pumpkin, but just as delicious for stews, stuffed, or soup. Give this Slow Cooker Pork and Pumpkin Stew a try for a warming weeknight meal.

Spaghetti: You’d never guess from its exterior that you can make a low-carb “pasta” with this squash. Halve it and bake, scoop out the seeds, then use a fork to scrape the flesh into strands. They’re like a blank canvas in terms of flavor so be creative in saucing them. You can go for the classic Spaghetti Squash with Light Marinara Sauce or go for more international flavor with a Spaghetti Squash “Ramen” Noodle Bowl.
All winter squash can be steamed, roasted, braised, sautéed, grilled, or turned into soup. You can also cook them together. Squash can take strong seasoning, so use your imagination to come up with bold herbs, spices, and condiments. And don’t forget to clean and roast the seeds to snack on or garnish soups, salads, and other dishes.
If you are still feeling a little overwhelmed by squash, check out the pre-cut produce section of your grocery store! Many stores offer precut squash ready to go. You can also check the freezer section for different types and cuts of different squash.