Eating more veggies has many health benefits for people with diabetes, and there is no better way to eat more veggies than with a clean green salad! Salads can be a great side dish or starter to a meal, but with the right components they can also take center stage and be a diabetes-friendly meal on their own. Read on to learn how to build the perfect salad to add to your meal plan!
Building blocks of a perfect salad

Greens: Every salad starts with a base of leafy greens, but there are lots of options out there! Light green lettuces like romaine or iceberg have the mildest flavor. Darker greens like spinach and kale are more nutrient dense, and have a stronger (sometimes bitter) flavor.
“Spring” or “baby” greens are darker greens that are picked when the plant is young, so they have a milder flavor. Try adding shredded cabbage or carrots to your greens for a little crunch, or arugula for a peppery taste.
Vegetables: Carrots, celery, cucumber, bell pepper, broccoli, tomatoes, onion, mushrooms, etc, etc.—almost any vegetable can be tossed into a salad. Experiment with whatever you have in your fridge!
Fruit: Fresh fruit adds a great burst of sweetness to any salad. Try chopped apples or pears for something mild and crunchy. Fresh berries, orange or grapefruit slices, pineapple, peaches, or grapes also make great additions.
Protein: Adding protein can turn a side salad into a satisfying meal. Cooked chicken, steak, or fish make great additions. For a meatless salad, add hard-boiled egg or beans like chickpeas, lentils, or cannellini beans.
Grains: Adding grains can give your salad an extra boost of protein and fiber, and add a chewy texture to balance the crunch of fresh veggies. Try something a little different like quinoa, barley, buckwheat, farro, or wheat berries.
Flavor boosters: Just a little bit of these can go a long way toward adding texture or flavor to your salad:
- Nuts and seeds like almonds, walnuts, pecans, pepitas, sunflower seeds, sesame seeds, etc. add a nice crunch.
- Dried fruit adds a chewy texture and nice burst of sweetness. NOTE: be sure to measure out how much you add – Just 2 level tablespoons of dried fruit like raisins or cranberries contains about 15 grams of carbohydrates.
- Something briny such as olives, pickled banana peppers, or capers can add a savory flavor. NOTE: Leave these out or use sparingly if you are watching your sodium! Briny foods like this are made with a lot of salt.
- Cheese can add a variety of textures and flavors, depending on the type of cheese. Try grated parmesan, crumbled feta, goat cheese, blue cheese, shredded cheddar or mozzarella.
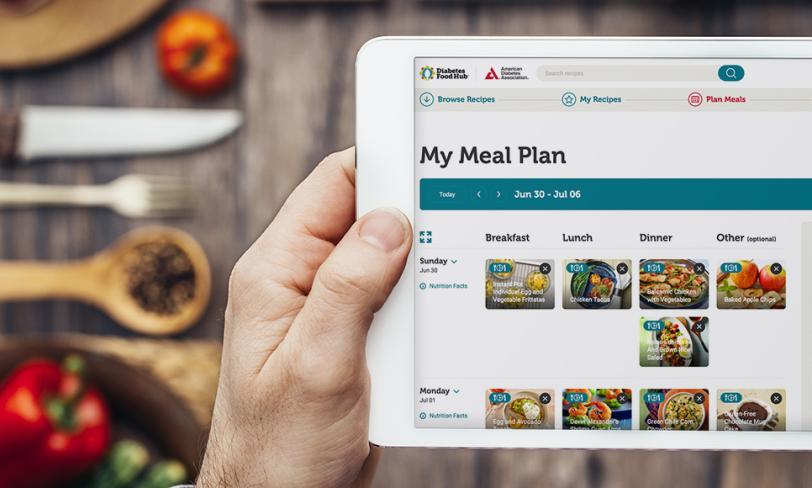
You can prep all of these ingredients ahead of time, and build a “DIY Salad Bar” in your own fridge! This is perfect for meal prepping, and makes it quick and easy to add more veggies to your meal plan.
Need more salad inspiration? Browse our salad recipes!
Dress it up!

Most people turn to the bottle when it comes to dressing their salad, but salad dressing is incredibly easy to make at home.
Bottled dressings can be surprisingly high in sugar and sodium, as well as other fillers and preservatives. When you make your own, you can control what goes in (and what stays out!).
A basic vinaigrette consists of 3 parts oil, 1 part vinegar, and a pinch of salt and pepper. If you like a tangier dressing, or want to cut down on the fat, try 2 parts oil to 1 part vinegar.
Blend your salad dressing by whisking the ingredients together in a bowl, shaking in a jar with a tight-fitting lid, or blending in a blender or food processor.
Here are some ideas for experimenting with your salad dressing:
Oil: Olive oil is the gold standard but other oils like canola, sunflower, or corn oil work just as well for a milder flavor. Nut oils like almond, pecan, or walnut oil add a nice nutty essence.
Vinegar: Any vinegar can work here – balsamic, red wine, apple cider, or rice – or you could try another acid such as lemon, or another citrus juice. Try puréed berries for something sweeter.
Other additions:
- Fresh or dried herbs like oregano, basil, thyme, or rosemary
- Minced fresh onion or garlic, or onion or garlic powder
- Dijon mustard or mustard powder
- Grated parmesan cheese
- Blend in an avocado, silken tofu, or tahini for a creamy dressing without the cream
- To add a little sweetness, try a dash honey, agave, or maple syrup