Diabetes management is more than just counting carbohydrates (carbs) and monitoring blood glucose (blood sugar) levels, it’s also making healthy decisions that fit your culture and traditions. Many cultural foods, such as tacos, pastas, stir-fries, and regional desserts, go beyond the food itself. They are often the focus when you celebrate holidays, birthdays, accomplishments, and so much more with friends and family.
However, these cultural foods may not always be the best choice if you are managing diabetes because of their carb, salt, fat, and sugar content. But with a few tweaks that can help you keep your blood glucose in your target range, you can still enjoy your favorites. Instead of thinking of these changes as a challenge, consider it an opportunity to try a different spin on traditional classics that will nourish your body and keep you healthy.
Tips for Healthy Eating with Culture in Mind
- Change them, don’t give them up: You don’t have to stop enjoying your favorite traditional foods if you live with diabetes. Make small changes that will make a big difference instead. For example, you can try:
- Using whole grain flour instead of white flour for breads or tortillas.
- Using lower-fat dairy products instead of high-fat varieties for foods like pasta sauce or masala.
- Including more non-starchy vegetables to increase a dish’s volume with little impact on blood glucose. You can also replace some carb-heavy foods in a recipe with non-starchy vegetables, such as making mashed potatoes with half potato and half cauliflower, or pasta with half noodles and half zucchini noodles.
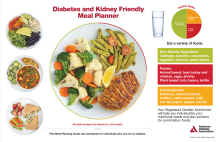
- Focus on balance: Make sure your meals include a balance of non-starchy vegetables, lean protein, and quality carbs to help manage your blood glucose. An easy visual tool to create balanced meals is the Diabetes Plate. Including a variety of non-starchy vegetables, like peppers, tomatoes, and leafy greens, like bok choy, chard, mustard greens, and collard greens in cultural dishes can increase the flavor and boost nutrients.
- Be aware of portion sizes: Cultural dishes can often be served family-style, meaning huge portions of each food are meant to be shared with everyone at the table. This can make it hard to manage your portions. Consider using a smaller or a pre-portioned plate to help you enjoy the food without having too much.
- Involve loved ones: Family and friends play a key role in diabetes management, especially when it comes to food and nutrition. Cooking together, sharing and creating new recipes, and discovering healthier options while grocery shopping can make making these changes enjoyable and comfortable.
- Welcome new traditions: Embrace the change! When you make healthy changes to the foods you love to fit your eating plan, you may be inspired to create new traditions that blend both culture and healthy choices. Don’t be afraid to try new herbs, spices, and different cooking methods to create new and exciting flavors for your favorite foods.
- Take the focus off food: For the events where the focus is on food, like the big meal on Thanksgiving, try instead to give your attention to the meaning of the event. Is it to gather with friends and family to share thanks for one another? To celebrate a milestone? Whatever the occasion or tradition, food should take second place to the intention of the gathering
Tying It All Together
Keeping culture alive while managing diabetes is possible through the power of small changes that make a big difference! By keeping the focus on culture and traditions, involving loved ones, and making healthy choices, you can continue to celebrate your heritage without giving up on your health goals. Remember, it’s about honoring traditions and supporting your health goals.
Don’t forget to sign up for Diabetes Food Hub’s e-newsletter for diabetes-friendly ideas and recipes.